- Messages
- 2,580
- Reaction score
- 87
Diving headaches have spoiled many dive trips. As there are different causes associated with headaches and diving, it can be as simple as your mask strap being overly tight or as complicated as a symptom of decompression sickness (DCS). Here are some common causes, preventions, and treatments for diving headaches.
Sinus headache
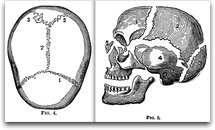
A sinus headache is caused by a sinus squeeze during ascents or descents. The symptoms are pain in the forehead, pain in the face, or pain in the cheekbone area. A diving headache caused by a sinus squeeze is due to the failure in equalizing pressure. Another cause is the inflammation of the sinuses or nasal cavity due to allergies or cold. Remedies include slowing your ascents and descents or using decongestants. However, its better not to dive if you are sick.
Tension headache
Symptoms of tension headache are pain in the head and pain in the back of the neck. Tension headaches are caused by muscle strain due to anxiety and muscular rigidity. Clenching your jaw during the dive can also cause tension headache. To prevent the development of muscle strain and consequently tension headache, you must learn to relax in the water. Eventually you will stop getting this type of headache if you dive within your abilities, gain experience, and become comfortable in the water.
Migraine headache
Symptoms of migraine headache include severe pain, visual changes, weakness or numbness of the arm, and nausea. Also post-dive vomiting is one of the migraine headache consequences, but if coupled with other symptoms could indicate a DCS hit. If the diver has a history of migraine headaches, there could be a direct correlation between diving and the onset of the cranial pressure.
Many of the medications used to treat migraines contain drugs which will increase the risk of nitrogen narcosis. Unless they are able to take measures for preventing migraine attacks, people with migraines should not dive. Anyone who suffers from migraine headaches and wishes to dive must consult a physician, preferably one with knowledge and experience in diving medicine.
Carbon dioxide toxicity headache
A dull pulsing head pain after diving is usually a symptom of this type of headache caused by carbon dioxide toxicity. This headache is caused by carbon dioxide build-up in the body. The increase in waste gas is usually due to hypoventilation (too little air intake). Hypoventilation usually happens when a diver doesnt take large enough breaths from his/her tank or doesnt breathe often. Simply put, not breathing enough to get rid of the carbon dioxide created in the body will eventually lead to this type of headache.
Carbon dioxide build-up is also caused by the usage of inefficient dive equipment, especially at depths below 30 meters (100 feet) where the gas density increases. This creates greater work of breathing, which leads to creating more carbon dioxide. Given that carbon dioxide is way more narcotic than nitrogen, sense dulling is a potential impact of excessive carbon dioxide build-up.
The best treatment here is to take slow, deep breaths to reduce the build-up. Also use high performance regulators with good flow characteristics. Carbon dioxide headaches dont respond well to pain relievers.
DCS headache
Headaches can also be a sign of DCS. DCS is caused by the formation of bubbles as dissolved nitrogen comes out of the tissues on ascent. DCS can lead to permanent physical impairment or death. Seek immediate medical attention if a diver complains of headache and has other signs of DCS like joint pain, swelling, skin rash, itching, dizziness, nausea, vomiting, ringing in the ears, or extreme exhaustion. A SCUBA diver is at risk of DCS when he/she does not decompress after long or deep dives before surfacing, or when he/she ascends too quickly or makes a panic ascent.
A word about dehydration
Dehydration is one of the most common problems, yet goes unrecognized. One of the first symptoms of dehydration is headache accompanied by dizziness, ranging from mild to severe.
The body uses fluids to maintain temperature. When the fluids go out, the body will concentrate fluids internally and peripheral flow is cut down. This in turn reduces the ability of the body to off-gas as the capillary exchange at the extremities became less efficient due to decreased circulation, which in turn invalidates all the decompression models. You may believe that you are off-gassing normally, whereas in reality, you are not. Watching your computer or following the tables wont help because the models are no longer valid. Also the blood flow to the brain is reduced due to dehydration, which results in reduced oxygen flow to the brain. Headache and dizziness occur accordingly.
It is advisable to drink at least two liters of water a day. When engaged in SCUBA diving, it should be increased to about four liters a day.
Sinus headache
A sinus headache is caused by a sinus squeeze during ascents or descents. The symptoms are pain in the forehead, pain in the face, or pain in the cheekbone area. A diving headache caused by a sinus squeeze is due to the failure in equalizing pressure. Another cause is the inflammation of the sinuses or nasal cavity due to allergies or cold. Remedies include slowing your ascents and descents or using decongestants. However, its better not to dive if you are sick.
Tension headache
Symptoms of tension headache are pain in the head and pain in the back of the neck. Tension headaches are caused by muscle strain due to anxiety and muscular rigidity. Clenching your jaw during the dive can also cause tension headache. To prevent the development of muscle strain and consequently tension headache, you must learn to relax in the water. Eventually you will stop getting this type of headache if you dive within your abilities, gain experience, and become comfortable in the water.
Migraine headache
Symptoms of migraine headache include severe pain, visual changes, weakness or numbness of the arm, and nausea. Also post-dive vomiting is one of the migraine headache consequences, but if coupled with other symptoms could indicate a DCS hit. If the diver has a history of migraine headaches, there could be a direct correlation between diving and the onset of the cranial pressure.
Many of the medications used to treat migraines contain drugs which will increase the risk of nitrogen narcosis. Unless they are able to take measures for preventing migraine attacks, people with migraines should not dive. Anyone who suffers from migraine headaches and wishes to dive must consult a physician, preferably one with knowledge and experience in diving medicine.
Carbon dioxide toxicity headache
A dull pulsing head pain after diving is usually a symptom of this type of headache caused by carbon dioxide toxicity. This headache is caused by carbon dioxide build-up in the body. The increase in waste gas is usually due to hypoventilation (too little air intake). Hypoventilation usually happens when a diver doesnt take large enough breaths from his/her tank or doesnt breathe often. Simply put, not breathing enough to get rid of the carbon dioxide created in the body will eventually lead to this type of headache.
Carbon dioxide build-up is also caused by the usage of inefficient dive equipment, especially at depths below 30 meters (100 feet) where the gas density increases. This creates greater work of breathing, which leads to creating more carbon dioxide. Given that carbon dioxide is way more narcotic than nitrogen, sense dulling is a potential impact of excessive carbon dioxide build-up.
The best treatment here is to take slow, deep breaths to reduce the build-up. Also use high performance regulators with good flow characteristics. Carbon dioxide headaches dont respond well to pain relievers.
DCS headache
Headaches can also be a sign of DCS. DCS is caused by the formation of bubbles as dissolved nitrogen comes out of the tissues on ascent. DCS can lead to permanent physical impairment or death. Seek immediate medical attention if a diver complains of headache and has other signs of DCS like joint pain, swelling, skin rash, itching, dizziness, nausea, vomiting, ringing in the ears, or extreme exhaustion. A SCUBA diver is at risk of DCS when he/she does not decompress after long or deep dives before surfacing, or when he/she ascends too quickly or makes a panic ascent.
A word about dehydration
Dehydration is one of the most common problems, yet goes unrecognized. One of the first symptoms of dehydration is headache accompanied by dizziness, ranging from mild to severe.
The body uses fluids to maintain temperature. When the fluids go out, the body will concentrate fluids internally and peripheral flow is cut down. This in turn reduces the ability of the body to off-gas as the capillary exchange at the extremities became less efficient due to decreased circulation, which in turn invalidates all the decompression models. You may believe that you are off-gassing normally, whereas in reality, you are not. Watching your computer or following the tables wont help because the models are no longer valid. Also the blood flow to the brain is reduced due to dehydration, which results in reduced oxygen flow to the brain. Headache and dizziness occur accordingly.
It is advisable to drink at least two liters of water a day. When engaged in SCUBA diving, it should be increased to about four liters a day.




![URL]](http://[URL]http://www.rlk.biz/ScubaImages/Skull_Sutures.jpg[/URL])

