I don't think there's anything to be gained by going to depth of relief on 1.6 ATA and a lot to be lost, so to speak, with the possibility of inert gas bubble growth, increasing tissue inert gas load and having a bent diver farther from help on the surface.
That is the great advantage of pure O
2. You don't need a computer or PhD to know that none of the tissues will be taking on diluent instead of giving it off.
I was at Ekofisk in the mid-1970s when a diver passed out (but still breathing) before getting in the chamber for his Sur-D-O
2 run. A tender jumped in with him and we drove him straight to 60'. A quick huddle and we took him off the O
2 mask and headed to 165'. He started to regain consciousness around 150'. He was fine after the half hour at 165' on air but got a little disoriented at around 80'. Crap, we didn't have any rich treatment mixes or a mix-maker onboard. We held at 75' for a quick huddle and decided to let him take five breaths off the O
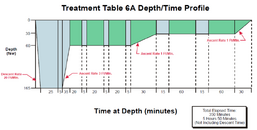
2 BIBs and five from the chamber. He started to show improvement after about 15 minutes so left him on the mask while moving to the 60' stop. We had no way of calculating if he took on too much Nitrogen so we added a 20 minute cycle to Table 6a at 60' and completed the run without incident.
Note: Green is breathing Oxygen and light blue is breathing air/chamber atmosphere
He was fine, but not a happy camper. Two other divers that week were hit a few hours after Sur-D-O
2 on the company's "new deep tables". A few heated minutes on the radio and he was on the next chopper to shore and the new tables were over the side. Yeah, that sucked. However it gave me an appreciation for the value of depth. The problem is that the majority of our treatment data is from hits after relatively short duration dives that are less than 200'.
How much treatment data do we really have for the 300'+ jumps that these rebreather warriors are doing?
Related Sidebar:
I was talking to a diver nearing his 30 year retirement from the Navy. He did a tour at EDU and was a guinea pig on some treatment table development dives. I asked him why they stopped at 60' instead of 66'/3 ATA. He said, "Simple, the gauges weren't accurate enough on fleet's chambers -- like +/-10' midscale". Yikes, I was ready for some great physiology insights.