DaleC
Contributor
If you're really serious about becoming proficient at pre-hospital emergency care (a good investment that will serve you and those around you your entire life) stick with the winners and practice/learn from those who are positive about what they do. It may appear cynicism is the new cool but it wears pretty thin, pretty fast. The key to success is not cynicism - it is curiosity.
Just to recap:
Forget survival rates, they don't mean anything to you as a care provider - statistics always break down at the individual level and when you provide care you are treating an individual, not a statistical average.
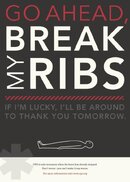
You do not break ribs every time you do CPR. The best thing you can do is gain access to a CPR-Doll with performance tracking capacity and practice practice practice until you can adequately and repetitively simulate a pulse. Not too hard, not too soft. You can't do it once during a course and expect to be good at it but if you do practice, it becomes somewhat like riding a bike.
Old bones heal too, just slower. As I said, I work as a rehab assistant in a complex care facility and deal with elderly fractures every day. It ain't pretty but it isn't the doom and gloom proclaimed by those so called experts.
Older people still have a lot to offer, if they choose and are able, and are not the drains on society some might suggest.
Just to recap:
Forget survival rates, they don't mean anything to you as a care provider - statistics always break down at the individual level and when you provide care you are treating an individual, not a statistical average.
You do not break ribs every time you do CPR. The best thing you can do is gain access to a CPR-Doll with performance tracking capacity and practice practice practice until you can adequately and repetitively simulate a pulse. Not too hard, not too soft. You can't do it once during a course and expect to be good at it but if you do practice, it becomes somewhat like riding a bike.
Old bones heal too, just slower. As I said, I work as a rehab assistant in a complex care facility and deal with elderly fractures every day. It ain't pretty but it isn't the doom and gloom proclaimed by those so called experts.
Older people still have a lot to offer, if they choose and are able, and are not the drains on society some might suggest.
Last edited by a moderator: