That is particularly true for monoplace (one-person) chambers, sometimes called torpedoes. The reason is the entire chamber atmosphere is usually nearly pure O
2, which is a much greater fire risk than during the
Apollo fire, which was at one atmosphere.
Here is an image of a monoplace from
Alert Diver Magazine, Q1 Winter 2015
View attachment 206083
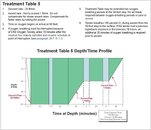
A multiplace chamber is preferred for treating DCS because treatments can be deeper than many monoplace chambers are rated for, Oxygen is administered by oral-nasal mask, and an attendant can be inside. That makes it possible to protect the patient from hurting themselves during an Oxygen convulsion, perform CPR if necessary, hang IV bags, take vitals for the hyperbaric doc outside, administer Oxygen if the patient is unconscious, and Oxygen exposures are usually much longer than most HOTs patients and separated by “air breaks”. For example:
- 60' for Table 5 & 6
- 165' for Table 4, 6A, & 7
- 225' for Table 8
Again, look at the chart of Table 5.
View attachment 206082
Air breaks are possible because the chamber atmosphere is air and the diver breathes from a
BIBS mask (Built-In Breathing System) when on O
2. Of course Oxygen levels, and therefore the fire hazard, on air alone is much higher than on the surface. Most (maybe all???) multiplace hospital chambers today use a BIBS mask with a demand regulator for supply AND exhaust. The exhaust is vented outside so the chamber atmosphere isn’t contaminated by even higher oxygen levels.
Many multiplace chamber operators allow divers to bring a book in with them because the fire risk is lower than a monoplane chamber filled with pure O
2. You will often see a sign like this near the entrance to a chamber:
View attachment 206081